Focus on Insulin Resistance
 The National Cholesterol Education Panel (NCEP) issued new guidelines on the prevention and treatment of high cholesterol in adults in May of this year. Changes in their newest ATP III report correctly put more emphasis on the risk of coronary heart disease due to insulin resistance and the metabolic disturbances associated with it. This insulin resistant condition is known as the metabolic syndrome, insulin resistance syndrome or simply Syndrome X.
The National Cholesterol Education Panel (NCEP) issued new guidelines on the prevention and treatment of high cholesterol in adults in May of this year. Changes in their newest ATP III report correctly put more emphasis on the risk of coronary heart disease due to insulin resistance and the metabolic disturbances associated with it. This insulin resistant condition is known as the metabolic syndrome, insulin resistance syndrome or simply Syndrome X.
What is insulin resistance? With insulin resistance, receptors on the body’s cells do not work properly. The cells are not letting insulin--and the glucose carried by insulin -- enter the cells’ walls. As a result, glucose or blood sugar tends to accumulate in the blood. This reduced sensitivity to insulin can initially be overcome by extra insulin output; however, when extra insulin cannot overcome this resistance, blood sugar levels rise.
Why is insulin resistance harmful? Type 2 diabetes mellitus (Type 2 DM) nearly always starts with insulin resistance. However, insulin resistance is associated with many metabolic disturbances that develop long before Type 2 DM or even blood sugar levels begin to rise above the normal range, including: • Increased risk of cardiovascular disease • Low HDL or “good cholesterol” levels • High triglyceride levels • More small, dense LDL or “bad cholesterol” particles that lead to atherosclerosis • Higher insulin levels • Increased tendency for blood clots to form The above metabolic changes lead to more atherosclerosis, even when total cholesterol is in the “desirable” range of 200 or less. Most patients with low HDL levels and elevated triglyceride levels do show evidence of insulin resistance.
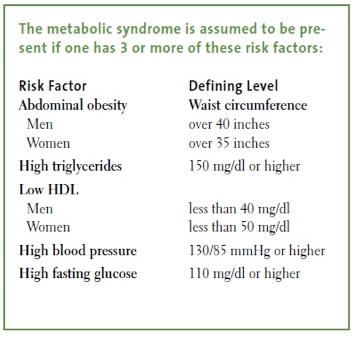
Detection of insulin resistance itself is not easy Unfortunately, there is no simple, cost effective test that directly measures the presence of insulin resistance itself. However, metabolic changes, such as an increased hip to waist ratio, low HDL and elevated triglycerides are easy to measure and can be used to predict its presence. The NCEP has established five risk factors, shown on page 97, for identifying the likely presence of the metabolic syndrome. Given the current problems in directly measuring and diagnosing insulin resistance, the use of the ATP III’s method of assessing the presence of the metabolic syndrome seems reasonable. All of these metabolic changes have been associated with an increased risk of a fatal heart attack or stroke. Clearly there is a need to diagnose and treat the metabolic syndrome whenever it exists. Waiting for Type 2 DM to develop or clinical signs of cardiovascular disease makes no sense. The most important strategies for reducing insulin resistance and the metabolic syndrome associated with it include eating a diet that is high in fiber and low in fat, sugar and refined carbohydrates. It is also important to exercise. See the box below for optimal strategies to prevent or reverse insulin resistance and the metabolic abnormalities associated with it.
 By Dr. James J. Kenney, PhD, RD, FACN. Dr. Kenney is the Nutrition Research Specialist for the Pritikin Longevity Center in Turnberry Aisle, Florida.
By Dr. James J. Kenney, PhD, RD, FACN. Dr. Kenney is the Nutrition Research Specialist for the Pritikin Longevity Center in Turnberry Aisle, Florida.
 By Dr. James J. Kenney, PhD, RD, FACN. Dr. Kenney is the Nutrition Research Specialist for the Pritikin Longevity Center in Turnberry Aisle, Florida.
By Dr. James J. Kenney, PhD, RD, FACN. Dr. Kenney is the Nutrition Research Specialist for the Pritikin Longevity Center in Turnberry Aisle, Florida.